Reno, age 64, starts prepping for Thanksgiving in October. Anything he can make and freeze in advance, he does: Apple pies. Peach pies. Butternut squash. The list is long, because he and his husband, John, feed a crowd.
“Every year we have an open house. We tell people: If you’re hungry, if you don’t have a place — whatever it is, come have a plate,” Reno says.
This Thanksgiving was special. Earlier in the fall, Reno had added palliative care to his health routine, including extra help with COPD symptoms. With that extra support, he was able to enjoy hosting more than he has in a long time.
“I actually feel good,” Reno says. “Palliative care has been a real game changer for me, and I hope it can be for other people too.”
> Ask about palliative care for you or a loved one.
A “life of five”
Before considering palliative care, Reno had become a master of toughing it out. For years, he’d been living with chronic obstructive pulmonary disease (COPD), a serious lung disease that can flare up easily, bringing on symptoms like breathlessness and pain.
“I should’ve bought stock in Tylenol, I was taking so much of it. But it just wasn’t helping,” Reno says.
He refers to those years as “living a life of five”: On a scale of one to 10, his pain was consistently a five. It was a struggle. But he didn’t think he had any other options.
“I just learned to deal with it and try to be happy with it,” Reno says. “I told myself: Other people have it worse.”
Then he had a fall at home, and wound up in the emergency room of the local hospital. The ER doctor took a look at his medical record, and suggested a more powerful pain medication. He was stunned at how much it helped.
“All of a sudden, not only did the pain from the fall go away, but the COPD pain was more tolerable. And I was able to breathe so much better,” Reno says.
As his pain went down and his oxygen levels steadily went up, the ER doctor turned to Reno with another suggestion: palliative care.
“Me? Palliative care?”
Today’s medical advances are helping us live longer with more and more illnesses, which makes the medical field of palliative care more and more crucial.
Palliative care specializes in the challenges of living with a chronic, serious illness. For example, it often gives patients more options for managing their symptoms: The ER doctor suggested it for Reno partly so he could have regular, expert access to the medication that was finally bringing him relief.
But since palliative care is still a relatively new field, many people don’t know about it — or assume it’s the same thing as hospice or end-of-life care (it’s not). As a result, when it first comes up in conversation, many people have the same reaction as Reno: fear.
“The ER doctor says ‘palliative care’ and I’m like, ‘Me? Palliative care? I’m a old tough Italian. I don’t need palliative care,’” Reno remembers. “I was scared. I don’t know why. I just was scared.”
Then again, for the first time in recent memory, he was able to imagine a future that wasn’t a “life of five.”
“I started to think about how, for that time in the ER, I had no pain or much less pain,” Reno says. “So I started to talk to my doctors about palliative care. I talked to HopeHealth. I talked to the place where I get IVIG. I talked to my pulmonologist and primary care doctor.”
With every conversation, he learned a little more about what palliative care is — and isn’t.
And in the end, all his health teams said the same thing: “They all agreed I should go on palliative care,” he says.
“It’s like having a coach”
This past fall, Reno and John met Alicia Patalano, NP, their go-to expert on Reno’s palliative care team.
Alicia comes directly to their home, eliminating the stress and hassle of yet another clinic visit. There, she’s been working with Reno to find the right type and dosage of medication for his symptoms. She’s also working with him and John on any lifestyle changes that could help prevent COPD flareups. Between visits, if Reno or John ever have questions or just need reassurance, it’s as simple as picking up the phone.
“I like knowing that a professional comes over every once in awhile to check on me. It helps me feel more level, more secure,” says Reno.
Alicia also helps them think about future care decisions, and more immediate plans for quality of life — like the precautions they’ll need to take as they prepare for a cruise to the Cayman Islands, the latest on Reno’s bucket list.
“Stress ends up being a large component of chronic illness. We can decrease that stress, which helps patients better manage their illness,” Alicia says. “Often, patients and families aren’t sure what questions to ask, or when to ask them, or who to ask them to. As palliative clinicians, we encompass all of those things.”
“It’s like having a coach,” says Reno. “I like knowing I have that.”
> Read: Hospital, clinic, home: Understanding the settings of palliative care
“I smile about it now”
As soon as Reno concludes Thanksgiving prep, he starts in on Christmas.
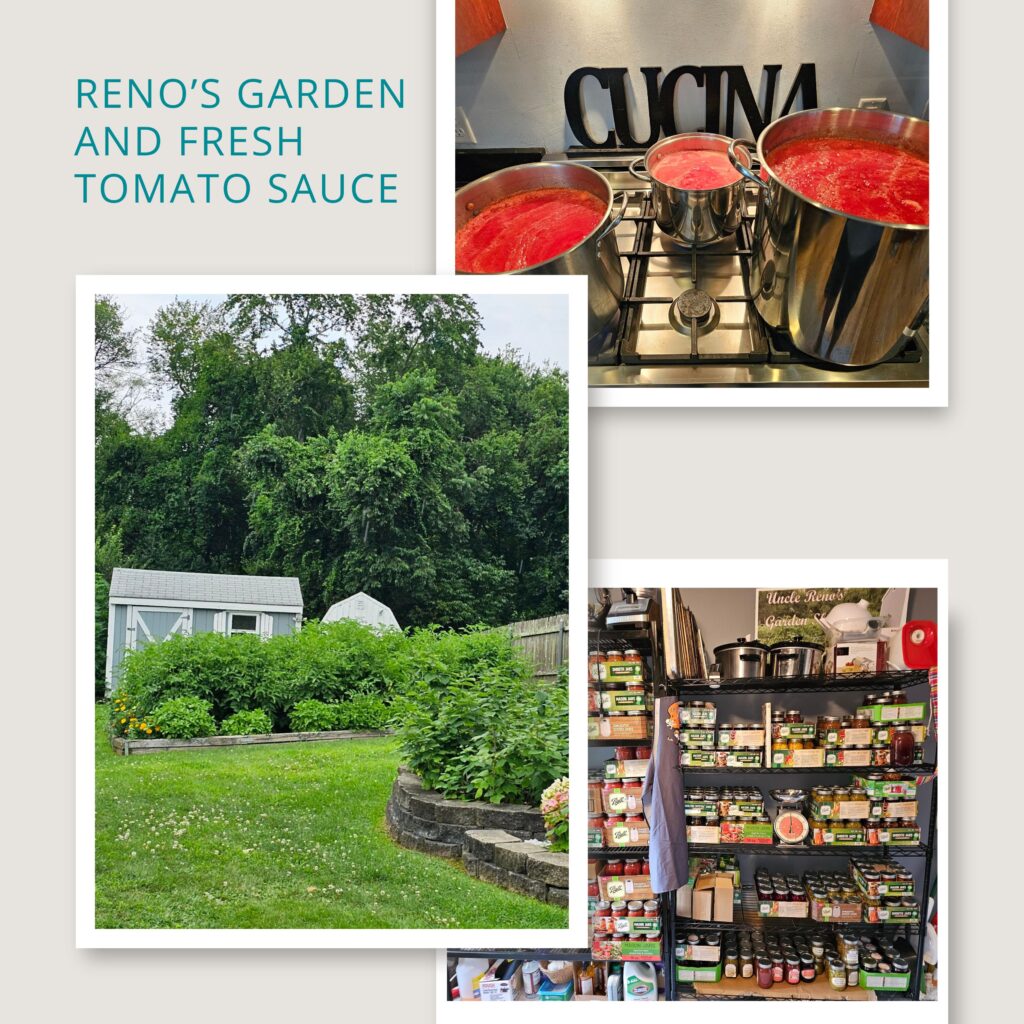
Every year, he and John fill gift baskets with preserves from Uncle Reno’s Garden Stand, which they run year-round from the front yard. John’s hot peppers recently had a banner harvest, so this season’s baskets have a “hot” theme: everything is spicy, from the salsa to the relish to the jam.
The weeks leading to this moment have been filled with peeling, cutting, spicing, stirring and canning. As always, Reno has presided over all of it. But for the first time in many years, he wasn’t battling with unmanageable pain.
“If I didn’t know about palliative care, I’d be where I was several months ago, feeling like I was going to die,” Reno says. “It was scary to start at first. I cried when I first heard about it. But I’m glad that I did. I smile about it now. I am still sick, but I feel better. The pain level is a lot more manageable. And it’s getting better every day.”

